Raise your hand if you have had or currently have back pain. Is your hand up? Studies suggest that approximately 80% of individuals will experience back pain at some point in their life and about 40% of individuals at a large gathering will currently be suffering from back pain. Translation: back pain seems to affect us all. In fact, back pain is the second most common reason individuals will see their doctor, trailing only the common cold. Unfortunately, we think about and treat back pain very differently than the common cold, with significantly more fear and anxiety surrounding the condition of back pain, when in all actuality, it is no more severe of a diagnosis. Like the common cold, the vast majority of cases of back pain will improve over time and do not require sophisticated or complex medical interventions. So why then do we worry if our back pain will get better or not when we do not seem to carry this same worry with respect to the common cold? The answer is we have not always taken the best approach to educating the population about back pain, leading to various misconceptions and myths that perpetuate unhelpful beliefs and behaviors. So let’s address some of the common myths about back pain.
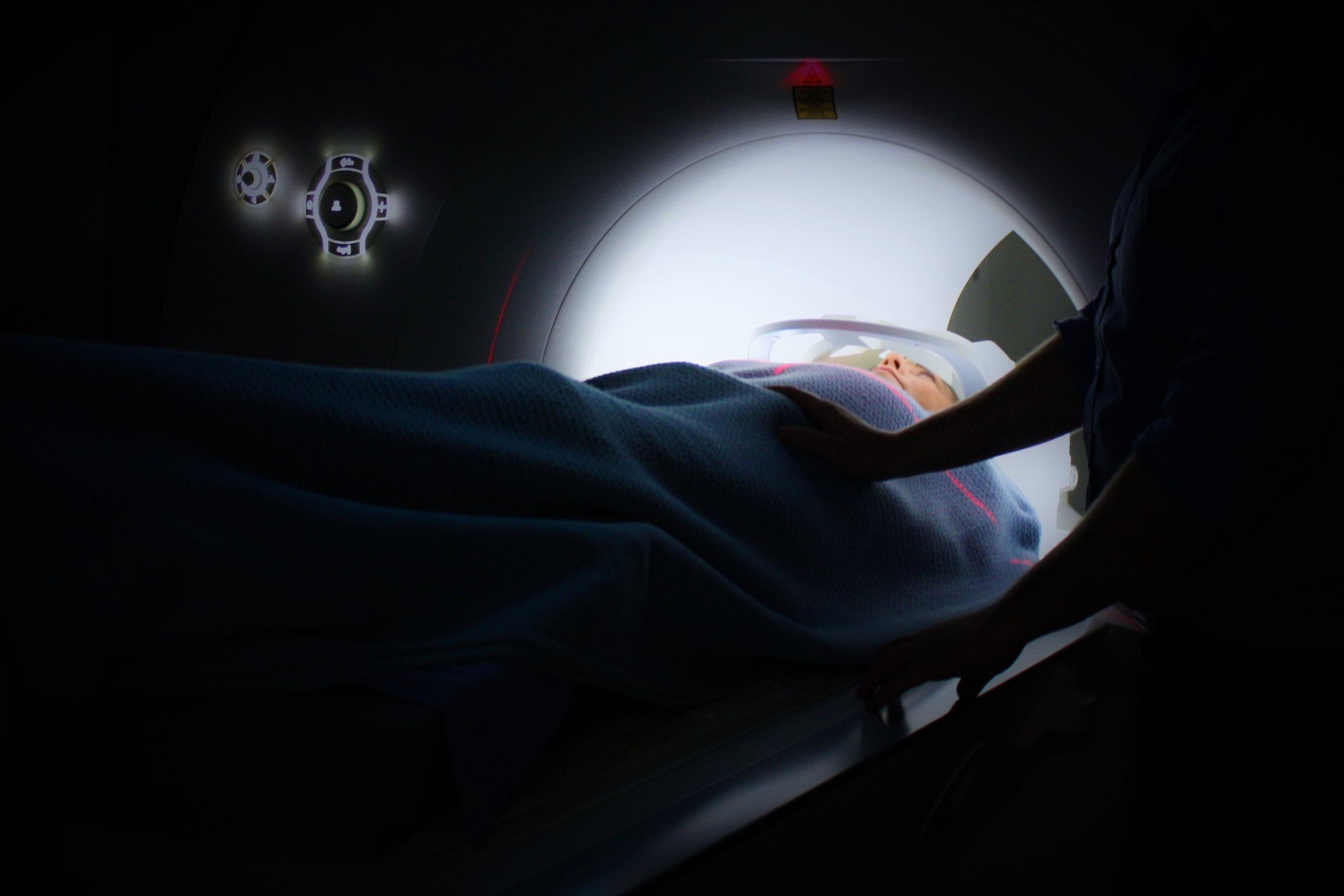
Myth: If my back hurts, I need an x-ray or an MRI in order to find out what is wrong so I can fix the problem.
Incorrect. It is very unlikely that the findings of an x-ray or MRI study will change the treatment strategy, unless the decision is whether or not to undergo surgery. In fact, x-ray and MRI findings have been shown to be poorly correlated with back pain. A deeper dive shows that approximately 40% of individuals WITHOUT back pain will demonstrate abnormal findings in x-ray and MRI studies. There is even some recent evidence that suggests individuals who receive x-ray or MRI studies early on in their recovery have worse outcomes than those who do not receive early x-ray or MRI studies. The fact is most cases of back pain will improve without expensive scans or complicated procedures. Education and exercise seem to be the keys to success.
Myth: My back hurts because I am old and have arthritis so there is nothing I can do about it.
False. Old age has not been linked with back pain. In fact, individuals between the ages of 30 and 50 have the highest rates of back pain. After the age of 50 your risk of back pain is actually slightly lower. Furthermore, most studies suggest that degenerative changes (i.e. arthritis) begin after the age of 30 and progress throughout our life span. So if arthritis always resulted in pain, why do individuals in their 30’s not have higher rates of back pain than individuals in their 70’s? The answer is because arthritis and back pain are not strongly linked and therefore not a scarlet letter one needs to carry with them or be fearful of.
Myth: I injured my back 10 years ago and I don’t think it ever quite healed.
Unlikely. Tissues heal. Most of the evidence suggests that bones, muscles, tendons, and ligaments completely heal after approximately 3-6 months. While the pain people experience can persist long after 3-6 months, that is not indicative that the injured tissue did not heal. Pain and injury are not one in the same. While it is true that most injuries carry with them pain, many individuals experience ongoing pain beyond the healing time of the injury they sustained. Why is this? Pain is an output of the brain and can be the result of an overactive nervous system. Pain functions to protect us from danger or potential threats in our environment. If we touch a burning hot stove, pain results in us removing our hand to avoid further injury to our skin. However, sometimes our nervous system protects us TOO much, sounding the alarm in the absence of something truly dangerous or threatening. Think of experiencing back pain from sitting or standing for 5-10 minutes. There are few cases where this is dangerous or inciting injury to tissues, but people often experience back pain with as little activity as this. This is most likely the result of an overactive or extra-sensitive nervous system, not an injury that never healed. So what can we do about this? Studies suggest education is the first line of defense. The more we know and understand about the science of pain, the less pain we tend to experience. Gentle exercise, activity modification, graded exposure, and pacing are also effective tools, all of which can be implemented by your physical therapist.
The take home message is if your back hurts there is usually something you can do to make it feel better without expensive scans or complex surgical procedures. There is good evidence for education, exercise, activity modification, ice, ergonomic adjustments, massage. The key is to take an active approach and to be patient, which is easier said than done. But the good news is the majority of cases of back pain will improve with time.